| No. | Viral Serology Tests | Sample | Volume | Rate | TAT |
| 1 | Dengue Antigen & Antibodies ( NS1 + IgG + IgM ) ELISA | Serum | 3 ml | 1500/- | 24hr |
| 2 | Rubella IgM ELISA | Serum | 3 ml | 500/ | 72hr |
| 3 | Measles IgM ELISA | Serum | 3 ml | 1200/ | 72hr |
| 4 | Herpes Simplex Virus 1+ 2 IgM ELISA | Serum | 3 ml | 600/ | 72hr |
| 5 | Varicella-Zoster IgM ELISA | Serum | 3 ml | 1200/ | 72hr |
| 6 | HEV IgM ELISA | Serum | 3 ml | 600/- | Every Thursday |
| 7 | HIV Ag & Ab ELFA | Serum | 3 ml | 500/- | 24hr |
| 8 | HCV ELFA | Serum | 3 ml | 500/- | 24hr |
| 9 | HBsAg – ELFA | Serum | 3 ml | 500/- | 24hr |
| 10 | HAV IgM ELFA | Serum | 3 ml | 600/- | 24hr |
| 11 | HBeAg ELFA | Serum | 3 ml | 600/- | 24hr |
| 12 | HBc IgM ELFA | Serum | 3 ml | 600/- | 24hr |
| 13 | Anti HBs Titre ELFA | Serum | 3 ml | 600/- | 24hr |
| No. | Molecular Tests | Specimen | Volume | Rate | TAT |
| Conventional PCR | |||||
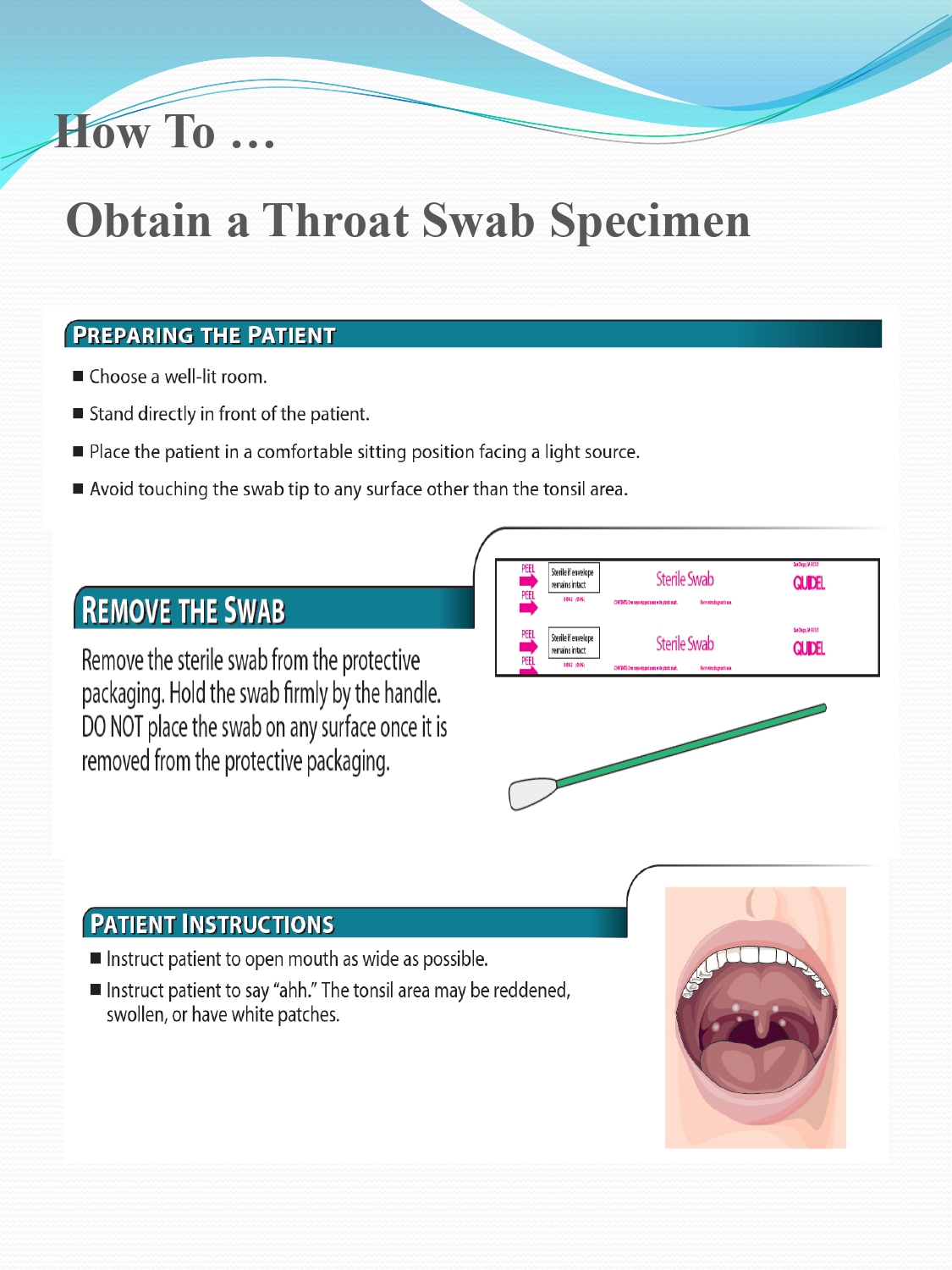
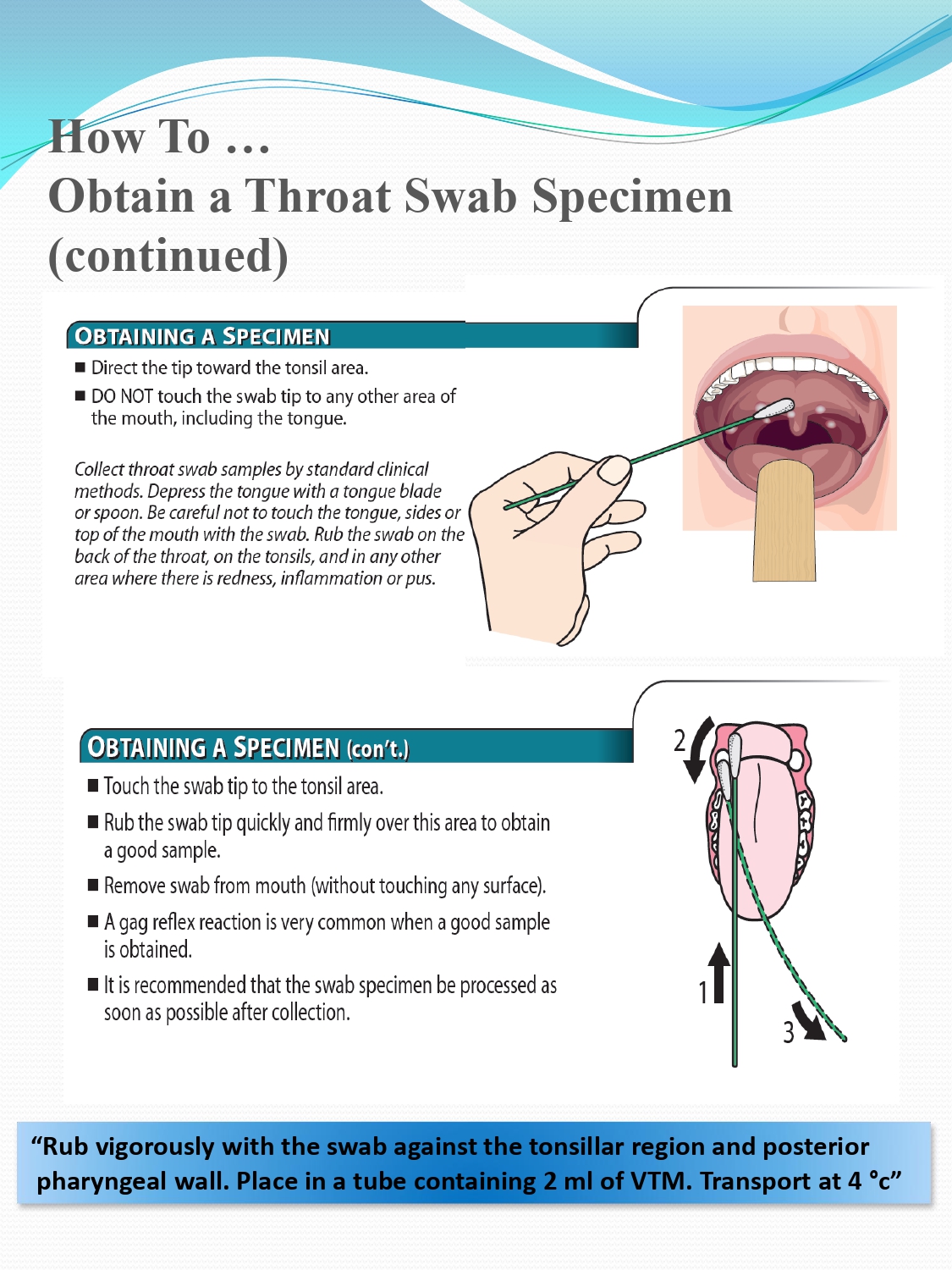
| 1 | Influenza A PCR | Throat Swab | VTM (3 ml) | 1900/- | 72hr |
| 2 | Respiratory Syncitial Virus PCR | Throat Swab | VTM (3ml) | 1900/- | 72hr |
| 3 | Herpes Simplex Virus 1 & 2 PCR | CSF | 1 ml | 2500/- | 72hr |
| 4 | Dengue PCR | Serum | 3 ml | 2500/- | 72hr |
| 5 | Dengue Serotyping PCR | Serum | 3 ml | 3500/- | 72hr |
| 6 | Rotavirus PCR | Stool | 3 ml | 2500/- | 72hr |
| 7 | Japanese B Encephalitis PCR | CSF, Plasma | 1 ml; 3 ml | 2500/- | 72hr |
| 8 | Varicella Zoster Virus PCR | CSF, Plasma | 3 ml | 2500/- | 72hr |
| 9 | Hepatitis B Qualitative PCR | Plasma | 3 ml | 2500/- | 72hr |
| 10 | Hepatitis C Qualitative PCR | Plasma | 3 ml | 2500/- | 72hr |
| Real Time Qualitative PCR | |||||
| 11 | Pan Enterovirus PCR (Polio virus, Coxsackie virus, Enterovirus, Rhinovirus, Echovirus) | CSF; Plasma; Swab | 1ml; 3ml; VTM (3 ml) | 3000/- | 72hr |
| 12 | Leptospira PCR | Plasma | 2500/- | 72 hr | |
| Real Time Quantitative PCR | |||||
| 13 | Hepatitis B Quantitative PCR | Plasma | 4750/- | 5 days | |
| 14 | Hepatitis C Quantitative PCR | Plasma | 5500/- | 5 days | |
The various ways of getting the services of the virology department follows (except for IP patients, as essential investigations are done as part of the work up)
Submitting specimens as Out Patients (OP)
Book a clinician at PMCH for op consultation and take a chart/file at the OP. As per the advice from the clinician the specimens to be submitted at the OP counter.
Submitting the specimen as By Hand OP (BHOP)
Call Pushpagiri Centre for Virology and get the details of test to be done, the kind of specimen to be collected, method of transportation etc. Bring the correct specimen in adequate amount with or without clinicians (outside/inside) prescription. Pay for the test at the OP billing counter and submit the specimen at the OP Lab Counter.
Alternatively, go to OP billing counter and pay for the test. Now go to the OP lab counter for specimen collection. Submit the specimen at the OP Lab Counter.
Collection of serum sample for routine serological tests
-
Draw 2mLof whole blood and transfer into red/plain tube needed.
-
Allow it to clot for 15-30 minutes at room temperature.
-
Centrifuge for at least 15 minutes at 2200-2500 RPM.
-
Pipette the serum or plasma into a clean plastic screw-cap vial and attach the label.
Collection of Plasma Sample for PCR
-
Draw 4mLof whole blood for each 2 mL plasma needed (EDTA /Lavender tube)
-
Invert it for 8-10 times for dissolving EDTA uniformly
-
Centrifuge for at least 15 minutes at 2200-2500 rpm.
-
Pipette the plasma into a clean plastic screw-cap vial and attach the label.
Place a clean wide mouth container (for example empty plastic container or a potty) in the toilet bowl or place a clean news paper or plastic wrap over the toilet seat opening (If the stool is very watery this may not be possible).
Pass the stool into the potty, plastic container or onto newspaper or plastic wrap.
Place small scoopfuls of the stool into the specimen container using the spoon built in to the lid of the specimen container (or the wooden stick, if supplied).Try to make sure that any parts of the stool which appear bloody, slimy or watery are put into the specimen container. If possible try not to mix urine with the stool sample – do not worry if this not possible.
Do not over fill the specimen container (the fill line indicates the required amount).Try not to spill the stool on the outside of the specimen container. If this happens clean the outside of the specimen container with soap and warm water, then wash your hands thoroughly with soap and warm running water and dry.
Put on the specimen container lid and screw on tightly. Wash your hands thoroughly with soap and warm running water and dry.
Dispose of the remaining stool in the potty, plastic container or newspaper in to the toilet.
If you have used a reusable container such as a potty, clean with your usual toilet cleaner. Ensure the potty is clean and dry before reuse. If you have used plastic wrap, newspaper or a disposable container, wrap these in newspaper then put in to a disposable bag and place in your outside bin.
Wash your hands thoroughly with soap and warm running water and dry.
Deliver to the OP Lab counter as soon as possible.
Results will be ready as per the turnaround time (TAT) mentioned above. Except Dengue, for all daily tests result will be despatched three times in a day viz. morning (9.30 am), noon (12.30 pm) and evening (3.30 pm). Dengue results will be despatched as evening report.
All results are despatched as per TAT. Hard copies will be send to Central Lab counter give. BHOP patient can collect the result by showing the test bill, from the Central Lab counter. Make sure that the results are ready by telephonic enquiry to virology laboratory, before coming to collect the results.
Alternatively apart from hard copies of results, BHOP patients can download the mobile app and get the electronic report also. For IP & OP patients in house electronic reporting is employed.
Hits: 492